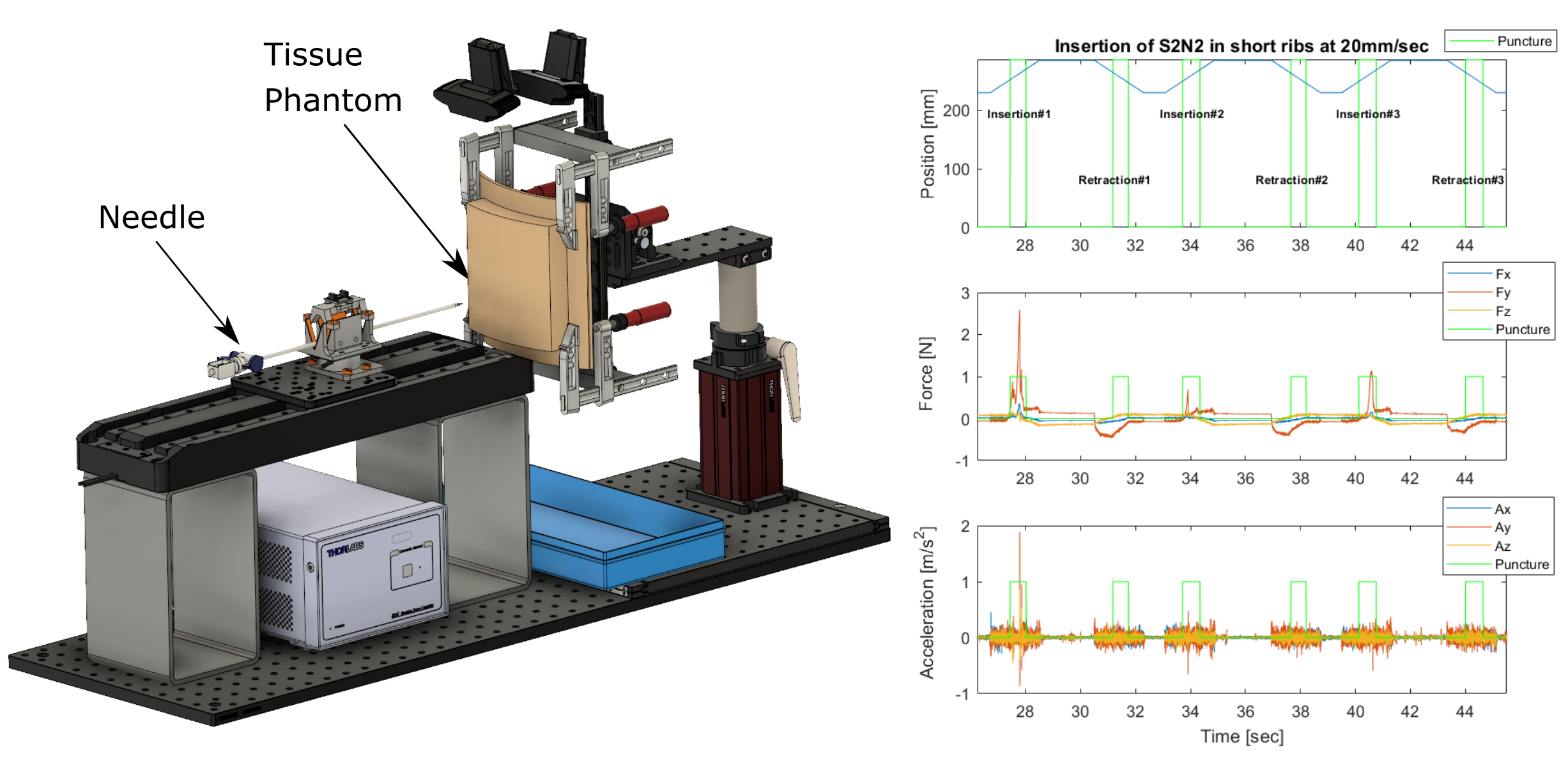
How much force is needed to puncture tissue? Sensors on the needle-insertion device (NID0) capture the needle position, force, and acceleration during insertions into and retractions from soft tissue phantoms and food-grade pork ribs.
Human soft-tissue properties vary widely: factors such as the patient's age and health can make enormous differences. As a result, junior medical professionals often have difficulty learning how much force is needed to cut through or puncture a particular type of tissue.
For example, during chest tube insertion, the doctor must use a needle to access the pleural space of the patient's body, puncturing through the pleural membrane but going no further. Surgeons typically perform these procedures blind, relying on a combination of anatomical knowledge and their sense of touch to guide the needle. Surgeons report feeling pleural punctures strongly in some patients, but not in others. Thus, even well trained surgeons may have difficulty, being limited by the resolution of their own human sensory organs.
Given these widely varying tissue properties, complications can occur for percutaneous subtasks within lifesaving procedures like chest-tube insertion. These complications occur more often with inexperienced medical professionals. An area of particular concern is that manually-inserted needles unintentionally perforate vital organs such as the lungs, spleen, and even the heart.
The development of realistic robotic training devices would allow surgeons to learn this difficult technique before their first real procedure. Augmenting their sense of touch via sensorized needles, or using such a needle to warn them of impending punctures, also has the potential to improve surgical outcomes.
In this research we measure tissue properties during needle insertions and will use this data to develop a predictive software model of needle-tissue interactions. We started by developing a custom needle-insertion device (NID0); preliminary experiments with it indicate that our force sensor is of sufficient quality, and we are currently in the process of developing predictive software models based on the captured data.
Ultimately our techniques should allow the development of robotic surgical-training devices that will react realistically (unlike current simulators and tissue phantoms), as well as sensorized needles that could augment a surgeon's sense of touch during a real insertion.
